Treating and preventing a compression fracture of the spine
A compression fracture
is a break in which the bone collapses. It can be caused by an injury
or tumors in the spine, but most compression fractures happen
because of osteoporosis, a disease that causes bones to weaken over time.
The most common compression fracture in people
with osteoporosis is a spinal compression fracture, also known as a vertebral
compression fracture. This kind of injury affects the vertebrae, the small
bones along the spine. Spinal compression fractures happen when there's too
much pressure on a fragile vertebra, causing the front of the bone to crack and
collapse.
Often, people with
osteoporosis experience a spinal compression fracture when they fall down, but fractures
can happen during everyday activities, such as reaching into a cabinet,
twisting during bathing, or sneezing.
Mild compression
fractures can cause minimal pain and a few other minor symptoms, but more
severe fractures can be extremely painful and damage the spinal cord.
Both men and women can
have a vertebral compression fracture, but women are at a much higher risk.
About 25% of postmenopausal women in the U.S. will have at least one fracture -- which, in turn, increases the risk of having another. More than 30% of people
who have a compression fracture of the spine will likely have another within a year.
Signs and symptoms of a compression fracture
Some spinal compression
fractures happen slowly. Small cracks can appear in the vertebrae and become
larger over time until the bone collapses. You might not know you have a fracture
until it's seen during a chest or spinal X-ray.
These slowly occurring
compression fractures of the spine often come with long-term symptoms
including:
- A stooped posture known as kyphosis
- Increased pain when sneezing or coughing
- Loss of height
- Minor back pain that feels worse with movement, especially standing or walking
- Tenderness around the fractured bone
Other spinal
compression fractures can happen suddenly and cause severe, stabbing pain that
can last for weeks or months. This pain is usually felt in the middle or lower
back, or sometimes on the sides or the front of the spine.
Compression fractures
that happen suddenly or slowly form over time can both become severe by putting
extra pressure on the spinal cord and nerves running down the spine. When this
happens, you might also have:
- Difficulty walking
- Loss of bladder or bowel control
- Numbness or tingling in the lower body
- Weakness
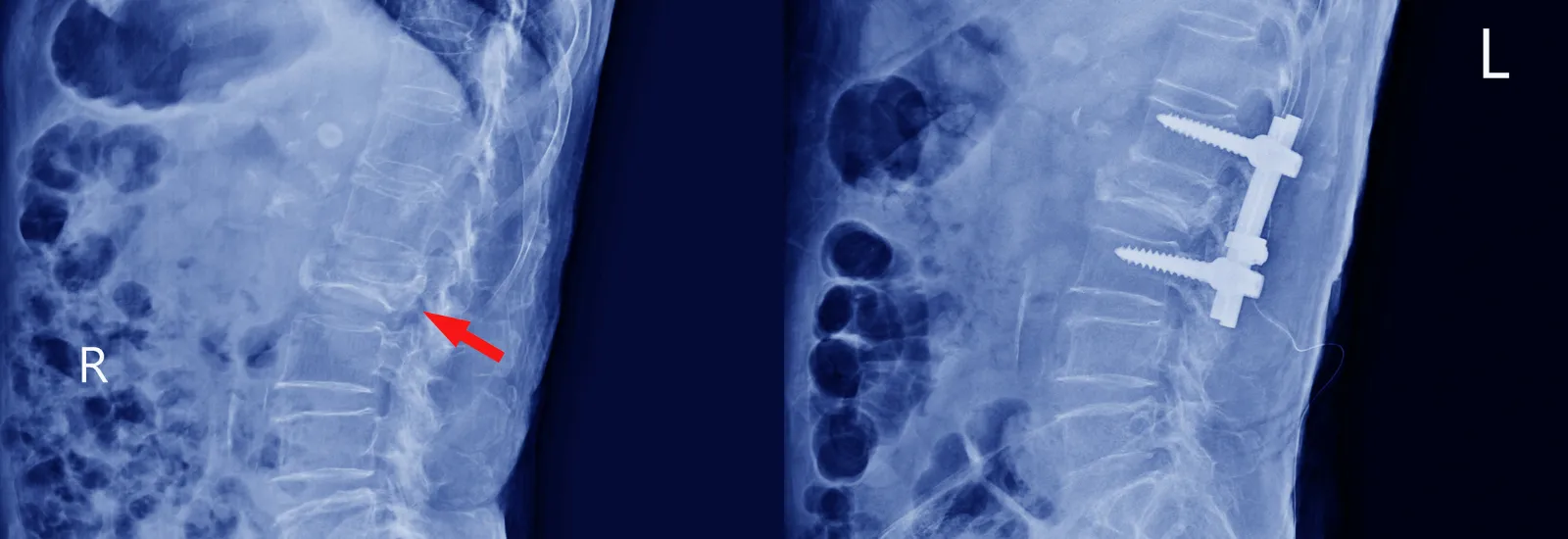
Diagnosing and detecting a compression fracture
Diagnosing a vertebral
fracture starts with a physical exam, during which your provider will ask
questions about your symptoms and medical history. You will likely need to
stand so your provider can see if your spine is straight, curved, or
stooped. They might also press different parts of your spine to help find the
location and cause of your pain, check for weakness or loss of sensation in
your lower body, and examine your reflexes.
If your provider thinks
you might have a spinal compression fracture -- or if they want to rule out other
possible conditions -- they can order imaging to get a clearer
picture.
Your provider might order
a dual-energy X-ray absorptiometry (DEXA) scan, a test that checks your bone
density. From the results, your provider will be able to see if you have
osteoporosis and how severe it is. This will help to decide which treatment
options are best for you.
Compression fracture treatment
Most compression
fractures heal within eight to 10 weeks with rest and pain medication. Your
provider might also recommend a back brace.
Physical therapy is often ordered to
help strengthen the core muscles to support the spine. A physical therapist might work with you on balance and posture to help prevent future falls.
Surgery might be needed
if you continue to have significant pain or other symptoms for more than two
months after starting nonsurgical treatments. Your provider may recommend an open spinal surgery or
minimally invasive spinal surgery depending on your symptoms and other factors.
Preventing compression fractures
The most important way
to prevent compression fractures is to prevent and treat
osteoporosis. It's not possible to reverse the damage, but you might be able
to help slow or prevent worsening osteoporosis with the following:
- Do routine, weight-bearing exercises
- Don't smoke
- Eat a healthy diet
- Limit alcohol
- Take prescribed medication to help prevent and treat osteoporosis
Using fall prevention strategies and participating in exercises can decrease your risk of falls and lower your risk of another compression fracture.
The specialists at Reid Health Comprehensive Bone & Joint
Center
are here for you. Request an appointment to learn more about
how we can help lower your risk of fractures and keep you healthy and active.

