Occupational Therapy

Our occupational therapists guide
children to reach their maximum potential and independence in all areas. The
"occupation" in occupational therapy refers to the meaningful activities that
fill a person's day, and for a child, their primary occupation is PLAY, thus,
the occupational therapists (OTs) at Reid will address skill development in the
context of play.
Occupational therapy is a broad
profession that can address most issues that are preventing a child from participating
in what they love. For example, an occupational therapist may address sensory
concerns when a child has difficulty participating in bath time. If a child
has difficulty keeping up in school the occupational therapist may assess the
child's functional vision skills. For a little one that is not yet
grasping or manipulating objects, the occupational therapist may focus on
developing a child's grasp and fine motor development, implementing
adaptive materials and/or splints as necessary to assist a child to reach their
goals. A child that has problems at mealtime may need to work on feeding with
their therapists, (often a collaboration between occupational and speech
therapy), to address deficits in oral motor coordination and sensory aversions.

To prepare for the occupational
therapy evaluation think about the daily activities that are difficult for you
and your child to manage. These difficulties will likely become the foundation
of your child's plan of care.
Milestones by Age:
0-3 Months
- Reflexive grasping of toys placed in hand
- Batting at objects dangled overhead
- Visually tracks toys within 12 inches from child's face
- Lifts head 45 degrees while on tummy, may be wobbly
3-6 Months
- Maintaining grasp on toy 30 seconds
- Bringing hands and toy to midline
- Sits with parent support
6-9 Months
- Starting to bang items together
- Ring sitting
- Begins to roll ball back and forth
- Beginning to use spoon
- Begins to hold bottle
- Clapping hands
9-12 Months
- Turns pages in a thick book
- Removes objects from containers
- Can pick up small items with pinch grasp
- Beginning to throw balls
12-18 Months
- Opens and closes containers
- Places objects in and out of containers
- Begins removing clothes
- Marks on paper with crayons
- Beginning to stack objects
18-24 Months
- Inserting shapes, simple puzzles
- Scribble on paper
- Spoon feeds independently
- Helps take clothes off
2-3 Years
- Dresses self with help.
- Will imitate drawing lines and circles on paper
- Builds a tower of 6-8 blocks
- Identifies need to use toilet
- Begins to pull up zipper
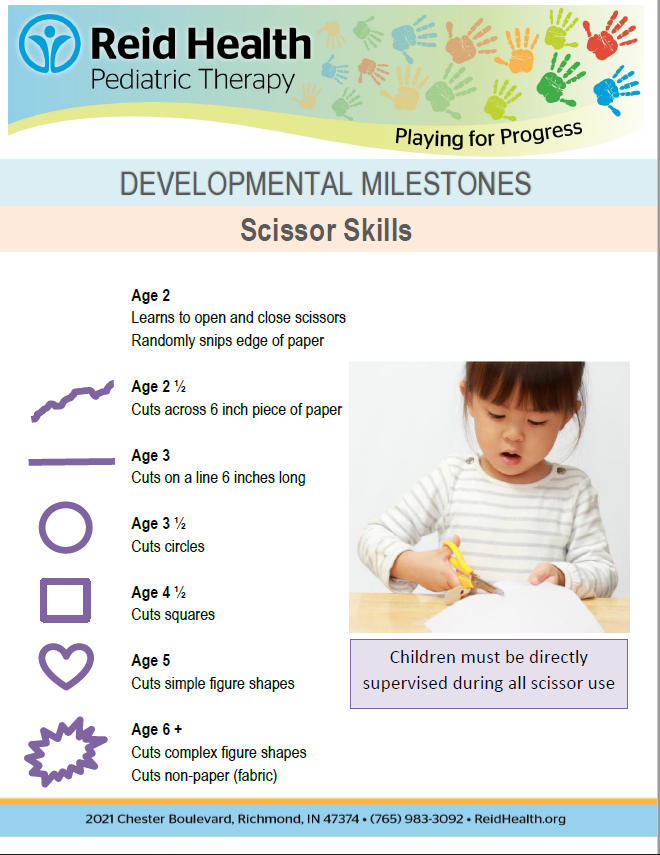
- Begins to use scissors with supervision (snipping paper)
3-4 Years
- Completes 4-5 piece interlocking puzzle
- Draws person (typically a head with limbs)
- Places bead on string
- Cuts lines and circles in paper
- Shows signs of dominant hand
- Uses fork and spoon independently
- Dresses self independently
- Toilet trained
5-6 Years
- Learning to tie shoes
- Completes up to 20 piece interlocking puzzle
- Writing numbers 1-10
- Completes cut and paste projects
- Cuts out intermediate figure shapes
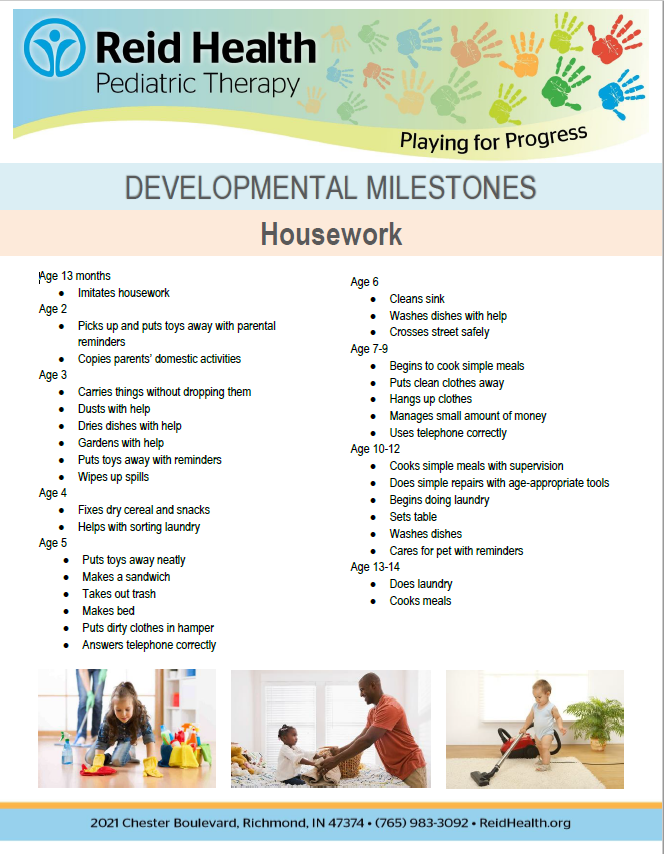
ADLs
Activities of Daily Living (ADL) refers to our essential
daily tasks. This is the foundation of what an occupational therapist will
address! The kids we see may have difficulty completing these necessary tasks
for many different reasons including deficits in motor skills, differences in sensory
processing, or difficulties with executive functioning/cognition. The pediatric
OTs at Reid will work to find the root cause of the obstacle and work with you
and your child to make lasting changes such as recommending modifications for
your environment or working with your child on activities and exercises to aid
their development of adaptive behavior.
Fine Motor and Grasping Skills

Fine Motor skills refer to the ability to perform
coordinated and precise movements needed for many common activities such as
pulling a zipper, picking up a coin, turning a screw, using scissors, or
stacking blocks. When a child has difficulty completing tasks of this nature,
there is often an underlying deficit in the strength of these small muscle
groups and a lack of coordination between the hands/fingers and eyes. Without
the necessary strength or coordination to perform fine motor activities, children
could be dependent on caregivers to complete daily tasks, such as dressing and
feeding. Deficits in fine motor coordination also typically contribute to
impairments in education tasks that involve handwriting.
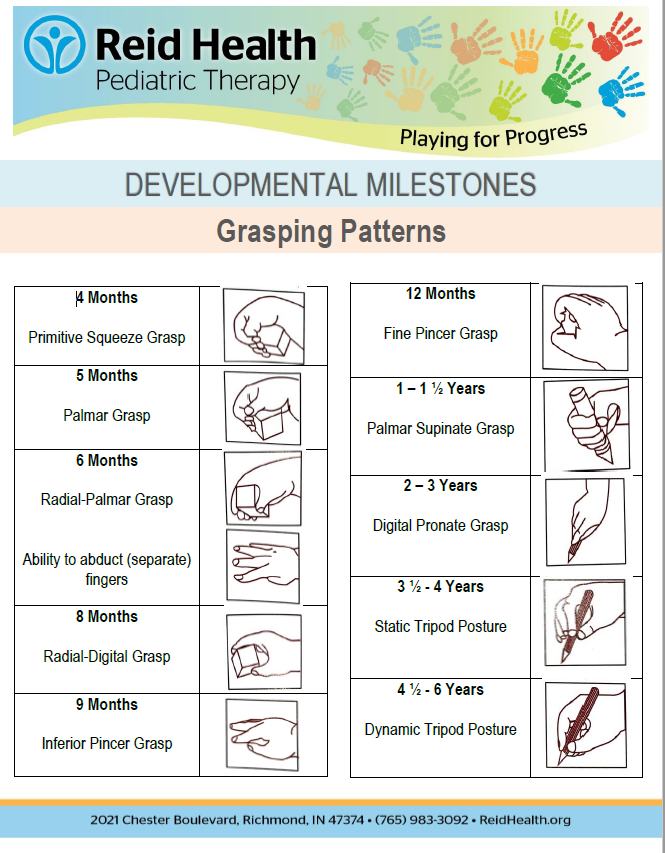
Delays in the development of age-appropriate grasping
patterns are one indication that a child may need additional help from an OT.
As a child grows and develops, there is a series of specific grasping patterns
that they will develop. Each grasp pattern plays a role in helping the child
complete more complex and dynamic activities.

OTs will work with your child to help develop the strength
or coordination necessary to develop age-appropriate grasp patterns and fine
motor skills. There is also the possibility to provide adaptive equipment
specific to your child's situation, such as built-up handles on writing
utensils or spring-loaded scissors, to make fine motor and grasping tasks
easier to perform.
Sensory Integration
Every single person has sensory needs and sensory preferences. We see this every day, people who like to snack or like to listen to music versus others who enjoy peace and quiet, some people enjoy roller coasters while others can't stand them. Preferences are normal, and in general, kids are more inclined to "seek" sensory input than adults, but when these preferences are paired with a strong emotional reaction (such as meltdowns), or cause us to act in unsafe ways (such as running, and crashing) it is appropriate to seek the help of an OT.

Many kids struggle with the processing of sensory information. Children may "seek" out additional input, this may look like: overexcitedly grasping all nearby objects, frequent spinning, or running and crashing into furniture. Children may also "avoid" certain types of input, which may look like: strong clothing preferences, frequently covering their ears to block out noises, or meltdowns during bath time.

The solution is not that these preferences "go away", but that the child develops adaptive behavior. Adaptive behavior may include asking for a wipe to clean their hands versus having a meltdown when they are messy at mealtimes. We work with families to provide kids with appropriate sensory input that helps to regulate their bodies throughout the day, so that there are fewer avoidance or seeking behaviors.
Functional Vision
Here at Reid we can complete
a screening of vision, this gives us information to know if further
recommendations are required. This can help to know if a child is plateauing
with progress due to vision problems, and treatments can be adjusted
appropriately. We often include visual perceptual activities in our treatments
to improve overall function. If vision deficits are present after assessment,
the OT will develop a specific treatment plan aimed at the needs of that
specific child that could involve environmental modifications, exercises aimed
to try and improve visual skills, and alternatives for meeting developmental
milestones in spite of visual deficits.
FES (Functional Electrical Stimulation)
The therapists at Reid have received training through
Restorative Therapies and are excited to treat our patients using the Xcite system,
which assists with proper motor sequencing during completion of functional
movement tasks and the RT300 iFES "bike" for arm, leg, and core activation
while benefitting muscle tone. Restorative Therapies is an Industry leader for
functional electrical stimulation, and these products are considered the
standard of care in neurological rehabilitation.
Functional electrical stimulation (FES) works by using
"safe, low-current electrical pulses to activate paralyzed or deconditioned
muscles for functional movement". While using the FES equipment our therapists
have the ability to stimulate up to 40+ muscle groups while engaging the
patient in a functional task. Both of these systems provide real-time
biofeedback and specific progressive resistive exercise (PRE) to recondition
weak or neurologically impaired muscles.
FES has
been cleared by the FDA to:
- Reduce muscle atrophy
- Reduce muscle spasms
- Improve local circulation
- Maintain or increase range of motion
- Facilitate muscle re-education
Pediatric therapy and Specialized Hand Therapy
Working as a collaborative team, our pediatric occupational
therapists and certified hand therapists can work together to help patients
with complex or post-operative diagnoses improve their function and quality of
life.
With collaboration and direction from each patient's
surgeon, immobilization protocols may be modified to include skilled and
functional therapy interventions throughout the healing process in order to
improve functional outcomes.
- Nerve grafts such as in brachial plexus surgery
- Hemiparesis
- Tendon transfers
- Trigger finger
- Replantation of digits
- Pediatric patients post orthopedic and/or neurosurgery
Splinting & Hand Orthotics
Hand splints are a therapeutic tool used to benefit a child's hand position to facilitate improved hand function. A splint may provide extra support to a weak joint or promote a neutral position to a hand with abnormal muscle tone.
In this photo, the child's thumb is splinted in a neutral position during weight bearing tasks. He is now getting the stretching and strengthening benefit of this activity that will lead to more balanced muscle tone throughout his affected limb. By crawling through his natural environment, with proper use of a splint, he is working on building a foundation to allow for more voluntary control of his hand.
Sometimes one size does not fit all. For kids with complex hand presentations, or with a goal to access something specific in their environment, a custom splint may be created. Our pediatric occupational therapists are skilled in creating adaptive devices to increase your child's comfort and independence.
Our therapists can work to find a splint that has a good
balance between stability and mobility to help your child reach their goals. This
may include ordering a pre-fabricated orthosis or creating a custom orthosis at
the clinic.
Constraint Induced Movement Therapy
This scientifically supported method
is considered one of the most effective treatment options for improving
function for a child with hemiparesis. Children with hemiplegia (impaired use
of one arm) often compensate for these deficits by completing tasks one-handed.
Left unaddressed, this unilateral approach to life will lead to permanent
changes in brain development and decreased independence with life skills. In constraint induced movement therapy (CIMT), a child's
unaffected limb is casted in order to reverse the symptoms of learned non-use
and promote increased functional movement of the affected limb during
functional play and everyday tasks. Patients that participate in CIMT show
improved bimanual abilities (the use of both hands) during desired tasks. The
high incidence of repetition in play strengthens neural pathways and leads to
increased independence in the child's natural environment.
- Cerebral palsy
- Traumatic brain injury
- Brachial plexus injury
- Other neurological diagnoses leading to unilateral upper extremity paresis
Myofascial Release
Myofascial refers to the
fascia of muscles, or the connective tissue that is interwoven throughout our
body. This tissue can become tight and restrictive preventing function,
mobility, and even circulation. Myofascial Release is a hands-on technique that
involves applying gentle sustained pressure to the connective tissue in the body
to eliminate pain, reduce tight muscles and associated spasticity, improve
blood/oxygen flow, restore/improve motion, and reduce overall body
tension. This technique has been found to be helpful in relieving symptoms
for many diagnoses such as chronic pain, migraines, fibromyalgia, anxiety, poor
posture, loss of flexibility, and for post-surgical rehab.
Specifically in children,
tension in the connective tissues in the body can cause children to become
easily agitated and upset for seemingly no reason. This tension can make it
difficult to physically participate in the child's meaningful and daily
activities. The therapists here at Reid can use myofascial release techniques
as a part of their treatment to release these tensions and make the child more
comfortable and willing to participate during the session and at home.
Wheelchair assessments
Occupational Therapy Common Diagnoses
- Prematurity
- Intrauterine drug exposure
- Feeding Difficulty
- Pediatric stroke
- Cerebral Palsy
- Traumatic Brain Injury
- Brachial Plexus Injury
- Orthopedic injuries
- Motor skill deficits
- Ataxia
- Developmental Delay
- Fine Motor Delay
- Autism
- ADHD
- Sensory Processing Disorder
- Down syndrome
- Rhett Syndrome
- Genetic disorders
- Life skills for young adults with developmental disabilities