Diabetes and surgery: What you need to know to prepare
3-minute read
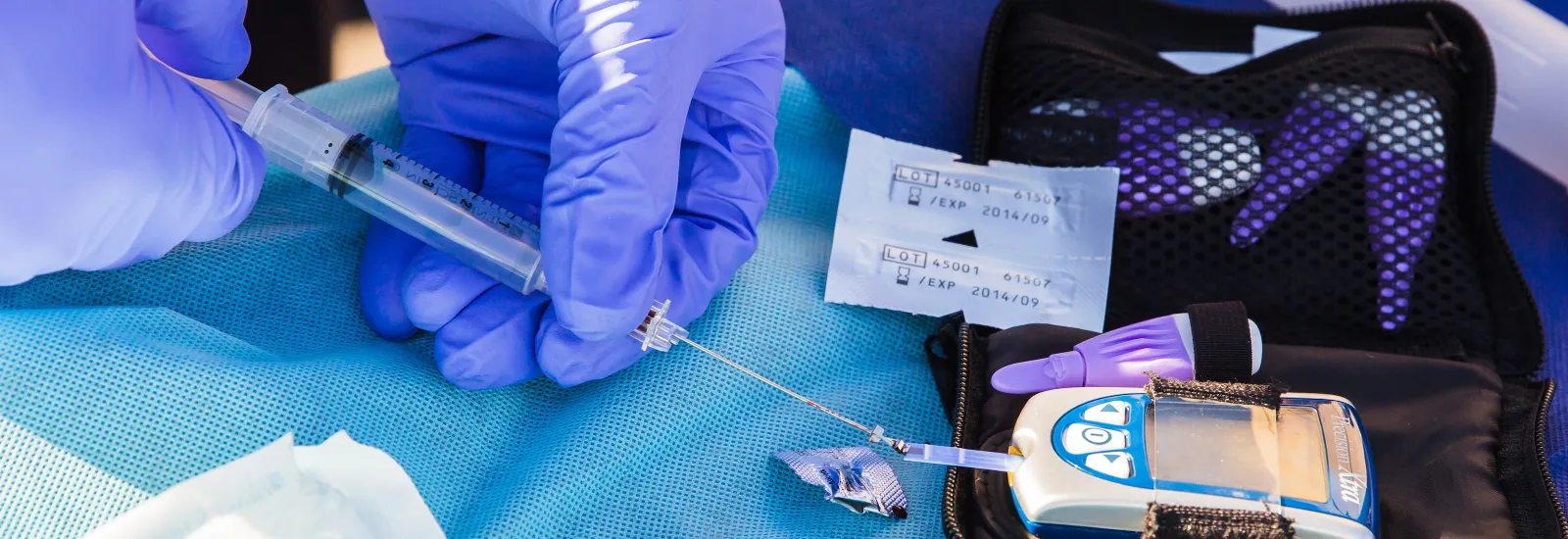
Everyone should be as healthy as possible before having
major surgery, but preparation is even more critical when you have diabetes. This
is because having a surgical procedure can negatively impact your blood sugar
(or blood glucose) levels, which can lead to complications. Structured
preparation for surgery or perioperative
programs, such as the
comprehensive program offered at Reid Health, can help people with diabetes who need surgery
understand the risks and take proper precautions.
Why following diabetes and
surgery guidelines is important
Having surgery puts strain on your body. Whether you have
been diagnosed with diabetes or have normal blood sugar levels, the extra
stress of surgery can cause your blood sugar level to increase.
If your blood sugar is too high at the time of surgery, it
can lead to complications during or after the procedure, including:
- Heart
and kidney problems
- Infection following surgery, especially at the surgery site
- Problems with fluids and electrolytes (minerals that help your nerves, muscles, heart, and brain function properly)
High blood sugar levels can also slow the healing process,
which might require a longer hospital stay.
For these reasons, your provider will check
your blood sugar before
surgery to ensure it's in the target range. In some cases, high blood sugar on
the day of the procedure can require your procedure to be delayed.
3 Steps to take before having
surgery
Your
healthcare provider will work with you before your scheduled surgery to help ensure
the best possible outcome. At Reid, your provider will refer you to the
Perioperative Clinic, where you will be evaluated to make sure your diabetes is
under control before your procedure. Your provider will also look for other health
issues that could lead to potential complications.
Before
surgery, your provider will work with you to come up with a plan and:
1. Talk to you about all the medicines
you are taking. If
you take metformin for Type 2 diabetes, your provider
might instruct you to stop taking it for 48 hours before and after surgery to
help avoid a complication called lactic acidosis. If you are on insulin treatment,
your provider will tell you what dose to take the night before or the day of
your surgery. You will also receive instructions for any other medications you take.
2. Review your recent blood sugar tests. Your provider will likely test it
again just before surgery. In some cases, you might need to meet with a
dietitian or follow a specific
meal plan during the week
before surgery to make sure your blood sugar stays well-controlled.
3. Discuss any diabetes-related
complications, as well as other health conditions, you might have. If you have experienced any problems
with your heart, eyes, or kidneys, or if you lose feeling
in your feet, your provider
might run additional tests.
You and your
provider can also discuss steps the surgical team will take during your
procedure to ensure your blood sugar remains in the target range. For example,
the anesthesiologist might need to administer insulin during the surgery.
What happens after surgery
Once your surgery is over, your blood sugar should be
checked frequently, either by you or your nurses. For some people, it can be
harder to control blood sugar after surgery due to factors such as:
- Being less active than usual
- Feeling pain — pain causes stress, which can increase blood sugar
- Having trouble eating
- Taking medicines that cause blood sugar levels to go up
- Vomiting — reduced fluids in your body causes blood sugar to be more concentrated
What to watch for during recovery
As you recover from your surgery, be alert to signs of
infection, such as fever and an incision that is hot to the touch, red,
swollen, oozing, or becoming more painful. If your recovery means you will be
in bed for a long period of time, remember to do all you can to prevent
bedsores. Having diabetes can cause you to have less feeling in your legs and
feet, and you might not know if you are developing a bedsore. Be sure to get up
as much as you can and shift your position in bed frequently.
In rare circumstances, having surgery can lead to serious
complications, such as diabetic ketoacidosis (DKA). You can get DKA as a result
of eating less than normal, getting an infection, or taking certain medicines. With
DKA, your body doesn't have enough insulin for cells to use blood sugar as
energy. Instead, the liver breaks down fat for fuel, which leads to the
production of acids called ketones. When too many ketones build up, you can develop
DKA.
DKA is a medical emergency and needs to be treated
immediately. Signs include:
- Achiness or muscle stiffness
- Being very tired
- Breath that smells fruity
- Dry mouth and skin
- Feeling very thirsty
- Flushing
- Headache
- Stomach pain
- Trouble breathing
- Urinating frequently
- Vomiting and inability to keep food or drinks down
If your blood sugar levels stay at 300 mg/dL or above or
you show signs of DKA, go to the emergency room or call 911.
If you are diagnosed with DKA, your treatment will likely
include:
- Receiving insulin, which can reverse DKA
- Replacing lost fluids, which can also help dilute excess sugar in your bloodstream
- Replacing electrolytes, which can become too low because of a lack of insulin
- Taking medications, such as antibiotics for infection
Reid Health providers are dedicated to helping you prepare
for all types of surgery. Get
more information or schedule an appointment with the Perioperative Clinic.

